Innovation
- a need for advancement
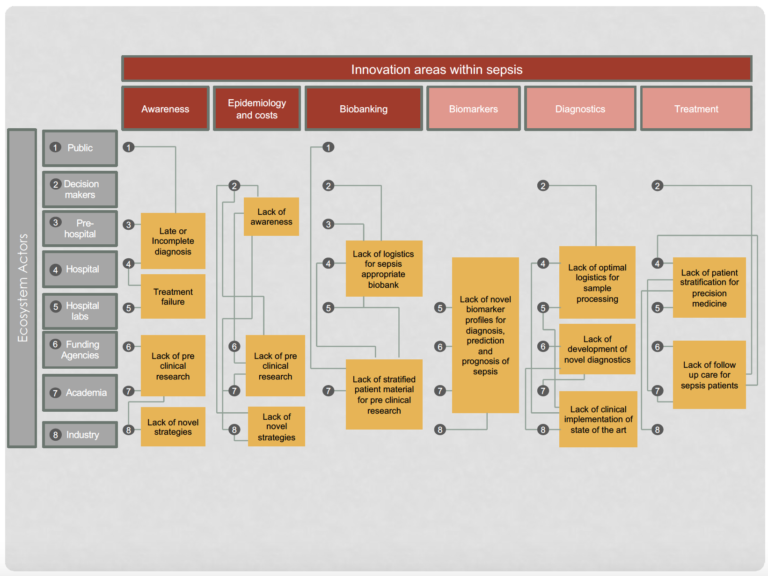
New collaboration interfaces and novel ecosystems are required in order to improve management of sepsis health care and drastically reduce sepsis mortality. To achieve this, we must mobilize a strategic interdisciplinary and intersectoral alliance focused on bringing about social, technical, medical, organizational and policy related innovations within sepsis. We have analyzed the current eco-system of actors and standards within sepsis care and identified critical lock-ins within the ecosystem, affecting key innovation areas (see image bellow). We are dedicated to catalyzing systems innovation and renewal of the ecosystem by focusing on the three following major problem areas within sepsis A) increase awareness B) decrease impact of antibiotics resistance and C) introduce precision medicine strategies.
Campaigning and Mapping
Increasing awareness of sepsis in Sweden is a prioritized goal for CombatSepsis. This also requires the quantification of the actual socioeconomic costs of sepsis both the acute disease but also the long-term negative effects and complications for sepsis survivors. Collectively, these efforts will confer benefits both at the level of individuals and at a societal level, where increased awareness will prioritize resource allocation to sepsis research.
Dampen effects of increasing antimicrobial resistance (AMR) in sepsis patients
Sepsis commonly originates from a local infection and antibiotics are the first line of treatment to limit the infection. The increasing incidence of AMR compromises, and will soon cripple, this treatment strategy, increasing the risk that life-threatening sepsis develops. When sepsis occurs, identification of the underlying pathogen and its antibiotic resistance pattern remains unacceptably long, despite significant progress in recent years. We aim to catalyze implementation of existing state-of-the-art diagnostic methods into current healthcare logistics within diagnostic labs, to facilitate the immediate handling of samples around the clock. Furthermore, we aim to develop novel treatments that complement or provide alternatives to antibiotics in two broad categories i) directly eliminate or weaken the underlying pathogen for existing treatments and ii) enhance or inhibit dysregulated components in the immune defence as determined by the underlying immune status of individual patients.
Introduce Precision Medicine in sepsis
Perhaps the most important factor to decrease mortality in sepsis is related to the introduction of Precision Medicine. Recent studies indicate that several of the sepsis treatment candidates developed by pharma industry that have failed in large population studies, may actually be effective in more narrowly defined subgroups. If successful, this novel paradigm will have far reaching consequence to “rescue” or “repurpose” failed treatments for particular patient sub-groups. The vision requires identification and implementation of improved stratification criteria of patients into treatable sub-groups combined with tools to monitor treatment success. Collaborative interactions will facilitate studies to create a biomarker defined stratification systems to target treatment to individual groups. The initial activities will be focused on addressing the following critical aspects:
- The rapid and dynamic stages of disease within sepsis patient groups should be incorporated into biobank design and implementation. Establishment of appropriate and well-documented biobanks linked to informative and adequate registers of patient data are of central, critical importance.
- At present, all sepsis patients receive similar therapeutic interventions due to limited opportunities to stratify patients. Stratification requires discovery and implementation of biomarker profiles using for example multi-omics, animal models of infection and well-characterized patient material. Such studies will deliver markers of immune system stage of disease, and the organ dysfunction profile in individual patients which will facilitate diagnosis and prognosis of patient sub-populations, paving the way for personalised medicine strategies.
- There is a critical need for treatment strategies tailored to counteract the long-term complications of sepsis. The biomarker profile of individual groups of patients will be monitored and linked to clinical data from patients attending post sepsis follow-up clinics. This will generate a unique and enhanced knowledge of the underlying molecular mechanisms contributing to long term complications and identify viable targets for generation of post-sepsis therapeutic intervention.